The short answer is Yes, Short-Chain Fatty Acids (SCFAs)—specifically butyrate, propionate, and acetate – have a profound and generally positive effect on the lungs and lung function.
This connection is known as the “Gut-Lung Axis.” It describes how the health of your gut microbiome directly influences your respiratory system.
Based on current research, here is the detailed breakdown of how SCFAs biologically upgrade lung health, the mechanisms involved, and the specific conditions they help manage.
1. The Biological Mechanism: How They Get to the Lungs
Since SCFAs are produced in the colon, you might wonder how they affect the lungs. The process involves three main pathways:
- Direct Migration: SCFAs are absorbed from the colon into the bloodstream. From there, they circulate systemically and can physically reach the lung tissue, where they are taken up by lung cells.
- Bone Marrow Priming: SCFAs travel to the bone marrow and “train” immune precursor cells (like macrophages and dendritic cells) before they even migrate to the lungs. This ensures that when these immune cells arrive in the lungs, they are less likely to be hyper-reactive (causing allergies/asthma) and better at fighting pathogens.
- Receptor Activation: Lung tissue is rich in specific receptors (FFAR2 and FFAR3) that are designed to receive signals specifically from SCFAs.
2. Key Benefits for Lung Function
A. Reducing Hyper-Inflammation (Asthma & Allergies)
One of the most well-researched benefits of SCFAs (especially butyrate) is their ability to calm an overactive immune system.
- Mechanism: Butyrate acts as a Histone Deacetylase (HDAC) inhibitor. In simple terms, it changes the way DNA is read in immune cells, effectively “switching off” the genes that produce runaway inflammation.
- Effect: It inhibits the activity of Type 2 Innate Lymphoid Cells (ILC2s). These are the cells often responsible for the exaggerated allergic response seen in asthma. By calming them, SCFAs reduce airway hyper-responsiveness (twitchiness) and mucus production.
B. Protecting Against Viral Infections (Flu & RSV)
SCFAs strengthen the lung’s antiviral defenses.
- Mechanism: Acetate has been shown to boost the production of Interferon-beta (IFN-β) in lung tissue. Interferons are signaling proteins that tell surrounding cells to heighten their antiviral defenses.
- Effect: Studies suggest that higher levels of circulating acetate can help the lungs resist viruses like RSV (Respiratory Syncytial Virus) and influenza by blocking viral replication and preventing severe lung damage.
C. Managing Chronic Conditions (COPD)
For Chronic Obstructive Pulmonary Disease (COPD), the anti-inflammatory nature of SCFAs helps prevent tissue destruction.
- Mechanism: In COPD, neutrophils (a type of white blood cell) often cause collateral damage to lung tissue while trying to fight smoke or pollutants. SCFAs modulate these neutrophils, reducing their destructive potential without stopping them from fighting bacteria.
- Muscle Wasting: Interestingly, some research suggests butyrate may help combat the muscle wasting (sarcopenia) often seen in advanced COPD patients, likely due to its systemic effects on muscle mitochondria.
3. Important Nuance: The “Propionate Paradox”
While SCFAs are overwhelmingly positive, high-level biochemical research has identified one specific context where balance is required.
- Bacterial Pneumonia: While SCFAs are great for viral defense and stopping allergies, very high levels of propionate (specifically when the ratio of propionate is much higher than acetate) might dampen the immune system too much in the face of certain bacterial infections like Staphylococcus aureus. The immune system needs a sharp inflammatory spike to kill these specific bacteria, and if SCFAs suppress that spike too heavily, the bacteria may persist longer. This is rare and usually linked to severe gut dysbiosis (imbalance) caused by antibiotic usage.
Summary of Benefits
| SCFA Type | Primary Lung Benefit | Mechanism |
| Butyrate | Reduces Asthma/Allergy symptoms | Inhibits HDACs; calms ILC2 immune cells. |
| Acetate | Fights Viral Infections | Boosts Type 1 Interferon response (antiviral shield). |
| Propionate | Reduces general airway inflammation | Modulates dendritic cells in bone marrow. |
Recommendation for Optimization
To maximize lung health via the gut:
- Prioritize Soluble Fiber: To produce these specific SCFAs, you need fermentable fibers like Acacia Fiber, inulin, pectin, and resistant starch (found in unripe bananas, cooked-and-cooled potatoes).
- Probiotic Strains: Look for Bifidobacterium and Lactobacillus strains, as they are key primary fermenters that produce the acetate and lactate needed by other bacteria to create butyrate.
Does SCFAs help with oxygen absorption in the lungs?
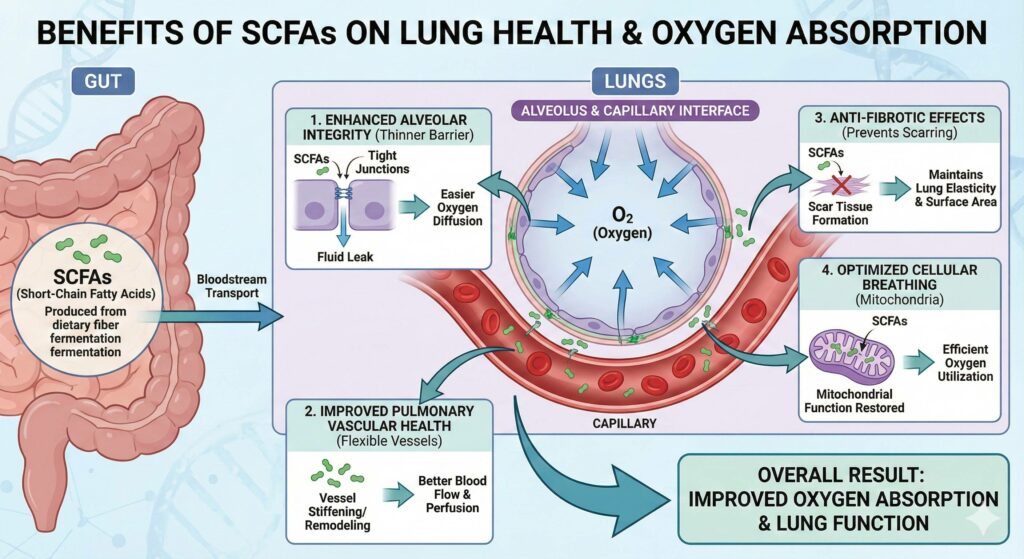
Yes, SCFAs help oxygen absorption, but they do it indirectly by repairing the “machinery” of the lungs rather than by changing the physics of oxygen itself.
You can think of it this way: SCFAs don’t make oxygen molecules “stickier,” but they clear the road so oxygen can get into your blood more easily.
Here is the detailed breakdown of how SCFAs (specifically butyrate) improve the efficiency of oxygen transfer from your lungs to your blood.
1. They Thin the “Barrier” (Improved Diffusion)
For oxygen to get into your blood, it must pass through a microscopic barrier called the alveolar-capillary interface. In many lung conditions, this barrier gets thick, scarred, or leaky, making oxygen struggle to cross.
- The SCFA Fix: Research shows butyrate strengthens the “tight junctions” (specifically proteins like ZO-1) between lung cells. This tightens the barrier, preventing fluid from leaking into the air sacs (pulmonary edema).
- Result: A drier, thinner, and structurally sound air sac allows oxygen to pass through instantly.
2. They Prevent Pulmonary Hypertension (Better Blood Flow)
Oxygen absorption relies on blood flowing smoothly past the air sacs to “pick up” the oxygen. If the blood vessels in the lungs are clamped shut (hypertension), oxygen absorption drops.
- The SCFA Fix: Studies (specifically in hypoxia models) have shown that butyrate prevents the remodeling and stiffening of pulmonary blood vessels.
- Result: By keeping lung blood vessels flexible and open, SCFAs ensure that deoxygenated blood can easily reach the air sacs to be re-oxygenated.
3. They Optimize “Cellular Breathing” (Mitochondria)
It’s not enough to just get oxygen into the blood; your cells have to use it.
- The SCFA Fix: Butyrate has been shown to restore mitochondrial function in lung tissue. Mitochondria are the parts of the cell that actually consume oxygen to create energy.
- Result: This ensures that the oxygen you do absorb is utilized efficiently by the lung tissue itself to stay healthy and repair damage.
Summary: The Oxygen Connection
| Mechanism | How SCFAs Help | Result for You |
| Alveolar Integrity | Tightens gaps between cells; reduces fluid leak. | Easier Diffusion: Oxygen crosses into blood faster. |
| Vascular Health | Prevents stiffening of lung arteries. | Better Perfusion: More blood reaches the air sacs to pick up oxygen. |
| Anti-Fibrotic | Stops scar tissue formation. | More Surface Area: Keeps lung tissue “stretchy” and usable for breathing. |
Immediate vs. Long-Term
- NOT an Immediate Bronchodilator: SCFAs will not open your airways instantly like a rescue inhaler (albuterol).
- Long-Term Remodeling: Their effect is structural and cumulative. They work over weeks and months to make the lung tissue healthier and more efficient at gas exchange.
Short-Chain Fatty Acids (SCFAs), particularly butyrate and acetate, serve as the biological foundation of the “Gut-Lung Axis,” directly influencing respiratory health by reducing systemic inflammation and structurally repairing lung tissue. By modulating immune responses, SCFAs help calm the hyper-reactive airways seen in asthma and COPD while simultaneously boosting antiviral defenses against infections like the flu. Crucially, they improve oxygen absorption not by altering oxygen itself, but by strengthening the “tight junctions” of the alveolar barrier and preventing the stiffening of pulmonary blood vessels; this creates a thinner, more efficient interface for gas exchange, ensuring that oxygen can diffuse rapidly from the air sacs into the bloodstream. It is critical to consume Soluble Fiber on a daily basis such as Acacia Fiber or Inulin Fiber.

Leave a Reply