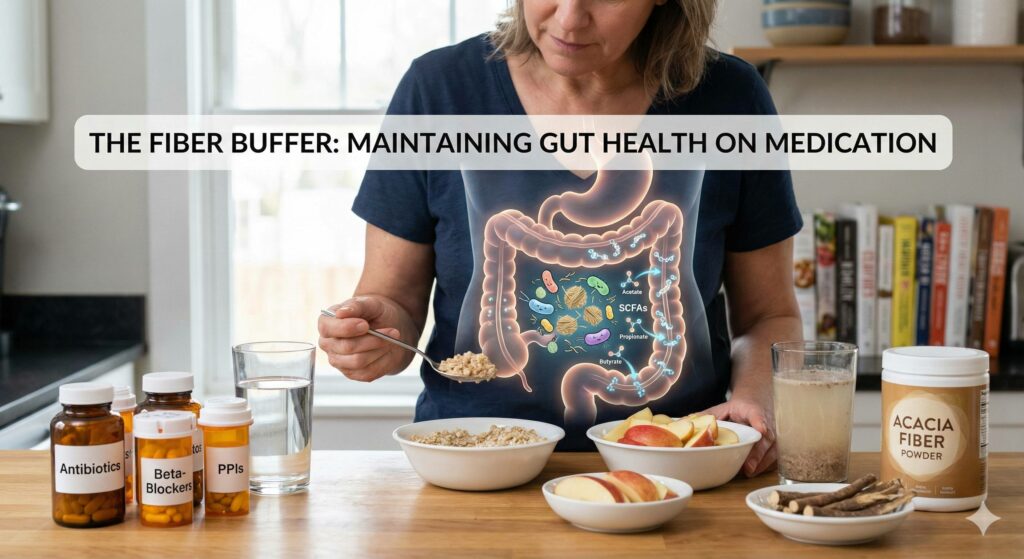
Research consistently shows that while certain medications can significantly deplete the beneficial bacteria responsible for producing short-chain fatty acids (SCFAs), adding soluble fiber to your diet acts as a “buffer” that can help maintain and even restore SCFA production.1
How Medications Disrupt the “Gut Factory”
When you take medications like proton pump inhibitors (PPIs), antibiotics, or beta-blockers, they don’t just affect their intended targets; they often change the chemical environment of your gut.2
- PPIs: Alter the pH of the digestive tract, allowing “upstream” bacteria (from the mouth and stomach) to migrate down and crowd out SCFA-producers.
- Antibiotics: Directly kill off large populations of beneficial microbes, leading to a “starvation” of the gut lining because SCFA levels drop.
- Benzodiazepines & Beta-blockers: Recent studies (late 2025) suggest these can leave long-term “fingerprints” on the microbiome, altering the competitive landscape for nutrients in the gut for years.3
Soluble Fiber: The Essential Substrate
If the gut is a factory, SCFAs (acetate, propionate, and butyrate) are the product, and soluble fiber is the raw material.4 Even if some of the “workers” (bacteria) are sidelined by medication, providing an abundance of raw materials can help the remaining beneficial bacteria work more efficiently.
1. Maintaining Anaerobic Stability
Medication-induced stress can increase the “redox potential” (oxygen levels) in the gut.5 Beneficial SCFA-producers are typically anaerobic (they hate oxygen).6 Soluble fiber helps maintain a low-oxygen environment, protecting these delicate microbes from being replaced by oxygen-loving, inflammatory bacteria like Proteobacteria.
2. Enhancing Resilience
Studies have shown that individuals on high-fiber diets experience less severe drops in microbial diversity when starting medication compared to those on low-fiber diets.7 The fiber essentially “feeds” the niche, making it harder for opportunistic pathogens to take over.8
3. Protecting the Mucus Barrier
When fiber is scarce, some bacteria will actually begin to eat the protective mucus lining of your gut for fuel. This leads to “leaky gut” and systemic inflammation. Adding soluble fiber ensures these bacteria have an external food source, sparing your intestinal lining.9
Practical Strategies for Maintenance
If you are currently taking necessary medications, you can support your SCFA production through these targeted dietary additions:
| Fiber Source | Primary Benefit |
| Inulin & FOS (Chicory root, onions, garlic) | Highly fermentable; specifically boosts Butyrate production. |
| Acacia Fiber | Gentle on the stomach; helps maintain a stable pH environment. |
| Pectin (Apples, citrus peels) | Forms a gel that slows drug transit time, potentially reducing GI irritation. |
| Beta-Glucans (Oats, barley) | Known to support the gut-heart axis by modulating bile acid recycling. |
Cautionary Note on Timing
While soluble fiber is beneficial, timing matters. High-fiber meals or supplements can sometimes interfere with the absorption of certain medications (like thyroid hormones or some heart meds) by binding to them in the gut.
- General Rule: Take your medications at least 1 hour before or 2-4 hours after consuming high amounts of soluble fiber.
Summary
While a wide range of common medications – including antibiotics, PPIs, and beta-blockers – can significantly disrupt the gut microbiome and deplete life-sustaining Short-Chain Fatty Acids (SCFAs), soluble fiber acts as a vital “raw material” to buffer these effects. By providing a substrate for beneficial bacteria to ferment, soluble fiber helps maintain an anaerobic environment, prevents microbes from eroding the protective mucus lining, and increases the overall resilience of the gut ecosystem. To maximize these benefits without compromising treatment, it is essential to focus on diverse fiber sources while carefully timing intake to ensure that fiber does not interfere with the absorption of necessary medications.

Leave a Reply