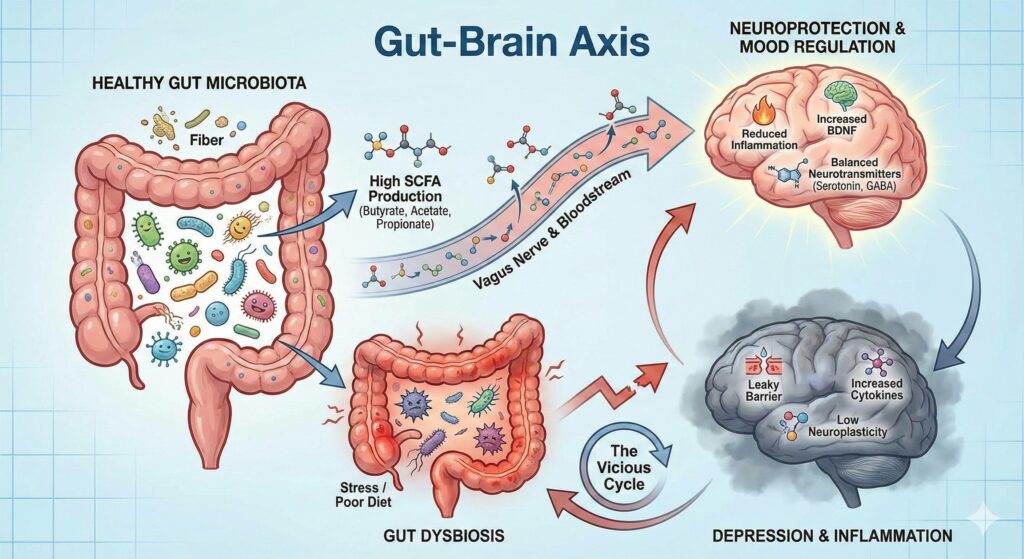
Recent research into the “gut-brain axis” offers a promising perspective on this question.
In short, Yes, Short-Chain Fatty Acids (SCFAs) can help with depression, and there is substantial evidence linking depression to gut dysbiosis. The relationship is less like a simple “symptom” and more like a bidirectional cycle – gut health affects mood, and mood affects gut health.
The following breakdown details the science behind SCFAs and depression, along with the connection to dysbiosis.
1. Can SCFAs Help with Depression?
Current research suggests SCFAs (specifically butyrate, acetate, and propionate) act as powerful antidepressants in the body. They are not sedatives; rather, they fix the biological “hardware” that allows your brain to regulate mood.
Here is how they work to alleviate depression:
- They Repair the “Leaky Brain” Barrier: Just as you can have “leaky gut,” you can have a “leaky brain-blood barrier.” When this barrier is weak, toxins enter the brain and cause inflammation. Butyrate helps repair this barrier, protecting the brain from inflammatory stress.
- They Reduce Neuroinflammation: Depression is increasingly viewed as an inflammatory disease of the brain. SCFAs inhibit the production of pro-inflammatory cytokines (immune signaling proteins) that make you feel lethargic and “down.”
- They Boost BDNF (Brain Fertilizer): SCFAs stimulate the production of Brain-Derived Neurotrophic Factor (BDNF). BDNF helps your brain grow new neurons and form new connections (neuroplasticity). Low BDNF is a hallmark of major depression.
- They Regulate Neurotransmitters: SCFAs influence the production of serotonin and GABA (the “calm” neurotransmitter) directly in the gut. Since about 90% of your serotonin is produced in the digestive tract, SCFA levels are critical for this supply chain.
2. Is Depression a Symptom of Gut Dysbiosis?
Technically, it is considered a comorbidity (a co-occurring condition) rather than just a symptom, but the link is so strong that many researchers view gut dysbiosis as a root cause for a subset of depression cases.
- The “Psychobiotic” Connection: People with depression consistently show lower levels of specific “good” bacteria (like Faecalibacterium and Coprococcus) that are responsible for producing SCFAs.
- The Vicious Cycle:
- Stress or poor diet causes Dysbiosis (imbalance of bacteria).
- Dysbiosis leads to lower SCFA production.
- Low SCFAs lead to inflammation and low serotonin.
- This causes Depression.
- Depression increases cortisol (stress hormone), which kills more good bacteria, restarting the cycle.
3. How to Increase SCFAs for Mental Health
Since you are interested in supplements and natural health, here are the most effective interventions studied for raising SCFA levels:
A. Direct Supplementation (Postbiotics)
You can supplement SCFAs directly, bypassing the need for fermentation.
- Sodium Butyrate: This is the most common form. It is often used for gut repair but shows promise for neuroinflammation.
- Tributyrin: A more advanced form of butyrate (a pro-drug) that is often better absorbed and reaches further into the colon than standard sodium butyrate.
B. Prebiotics (The Fuel)
The most natural way to boost SCFAs is to feed the bacteria that make them.
- Inulin & FOS: Soluble fibers found in chicory root and Jerusalem artichokes.
- Acacia Fiber: A gentle fiber that significantly increases butyrate production.
- Partially Hydrolyzed Guar Gum (PHGG): well-tolerated and effective for increasing SCFA levels.
C. Probiotics (The Factories)
- Look for “Psychobiotics” – strains specifically studied for mental health. The most effective SCFA-related strains usually include Bifidobacterium longum and Lactobacillus rhamnosus.
Summary Table: SCFAs vs. Depression
| Mechanism | How SCFAs Help | Result |
| Inflammation | Stop immune cells (microglia) from attacking brain tissue. | Reduces “brain fog” and fatigue. |
| Plasticity | Increase BDNF levels. | Helps the brain “rewire” itself out of negative thought patterns. |
| Gut Barrier | Tighten junctions in the gut lining. | Prevents toxins (LPS) from entering the blood and depressing mood. |
Short-Chain Fatty Acids (SCFAs) like butyrate play a crucial role in alleviating depression by repairing the blood-brain barrier, reducing neuroinflammation, and boosting critical mood-regulating compounds such as serotonin and Brain-Derived Neurotrophic Factor (BDNF). Depression is strongly linked to gut dysbiosis, often functioning as part of a bidirectional cycle where an imbalance of gut bacteria leads to low SCFA production, which fuels inflammation and depressive symptoms that, in turn, further degrade gut health. By restoring this balance through direct supplementation (postbiotics), fiber (prebiotics), or specific bacterial strains (psychobiotics), individuals can effectively target the biological roots of this “gut-brain” dysfunction to improve mental well-being.

Leave a Reply