Yes, substantial evidence suggests that Type II Diabetes (T2D) is strongly linked to gut dysbiosis and a subsequent deficiency in Short-Chain Fatty Acids (SCFAs).
Research increasingly views the gut microbiome not just as a bystander in diabetes, but as a driving factor. In many cases, low production of SCFAs (specifically butyrate, propionate, and acetate) acts as a “metabolic brake” that fails to engage, leading to higher blood sugar and insulin resistance.
Here is the breakdown of the biological mechanisms connecting T2D, dysbiosis, and SCFAs.
1. The GLP-1 Connection (The “Natural Ozempic” Mechanism)
One of the most critical roles of SCFAs is stimulating the release of GLP-1 (Glucagon-like peptide-1). GLP-1 is the same hormone mimicked by popular diabetes drugs (like Semaglutide).
- The Mechanism: When you consume prebiotic fiber, gut bacteria ferment it into SCFAs (mainly acetate and propionate). These SCFAs bind to specific receptors (FFAR2 and FFAR3) on the surface of enteroendocrine L-cells in your colon.
- The Result: This binding signals the L-cells to release GLP-1.
- The Impact on Diabetes: GLP-1 increases insulin secretion, slows gastric emptying, and improves satiety.
- Dysbiosis Link: If you lack the bacteria that produce SCFAs, your body produces less natural GLP-1, making it harder to manage blood glucose levels.
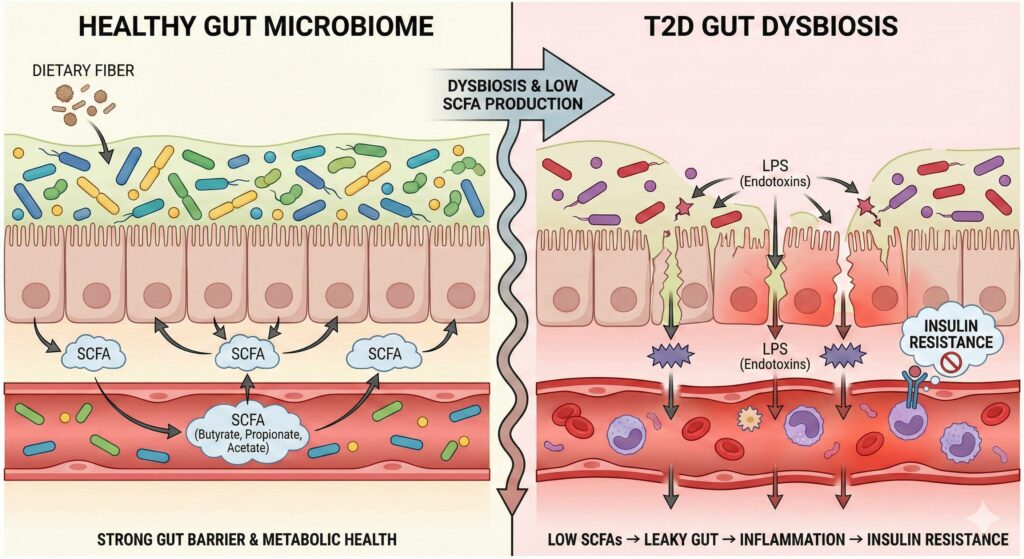
2. The “Leaky Gut” and Inflammation Loop
Type II Diabetes is often described as a state of chronic, low-grade inflammation. Low SCFA production is a primary cause of this inflammation.
- Butyrate’s Role: Butyrate is the primary fuel source for the cells lining your colon (colonocytes). It keeps the gut barrier tight and impermeable.
- The Leak: When butyrate production is low (due to dysbiosis), the gut barrier weakens (“leaky gut”). This allows Lipopolysaccharides (LPS) – toxins from the cell walls of harmful bacteria – to leak into the bloodstream.
- Metabolic Endotoxemia: The immune system attacks these toxins, causing systemic inflammation. This inflammation blocks insulin receptors on your cells, directly causing insulin resistance.
3. Hepatic Gluconeogenesis (Liver Glucose Control)
The liver creates glucose (sugar) when you are fasting (gluconeogenesis). In T2D, the liver often overproduces glucose, keeping fasting blood sugar high.
- Propionate’s Role: The SCFA propionate is absorbed into the portal vein and travels to the liver. It has been shown to inhibit the enzymes responsible for creating new glucose, effectively telling the liver to “turn down” sugar production.
The “Diabetic Microbiome” Profile
Studies have identified a specific dysbiosis “fingerprint” common in T2D patients. It is characterized by a loss of diversity and a specific reduction in butyrate producers.
| Beneficial Bacteria (Often Low in T2D) | Function |
| Faecalibacterium prausnitzii | Major butyrate producer; anti-inflammatory powerhouse. |
| Roseburia intestinalis | Converts dietary fiber into butyrate; supports gut barrier. |
| Eubacterium rectale | Key butyrate producer associated with insulin sensitivity. |
| Akkermansia muciniphila | Strengthens the mucus layer; inversely correlated with obesity and diabetes. |
Conversely, T2D patients often have an overgrowth of “opportunistic” pathogens (like Escherichia-Shigella) or bacteria that produce Branched-Chain Amino Acids (BCAAs), like Prevotella copri, which have been linked to insulin resistance.
Summary
Type II Diabetes can indeed be considered a sign of gut dysbiosis. The lack of SCFAs creates a triple threat:
- Reduced GLP-1 (lower insulin response).
- Increased Permeability (inflammation-driven insulin resistance).
- Unchecked Liver Glucose (higher fasting blood sugar).
Type II Diabetes is increasingly recognized as being driven by gut dysbiosis and a chronic deficiency in Short-Chain Fatty Acids (SCFAs). When the microbiome lacks specific fiber-fermenting bacteria, the body loses three critical metabolic controls: the stimulation of GLP-1 (which enhances insulin secretion), the regulation of hepatic gluconeogenesis (preventing the liver from overproducing sugar), and the maintenance of a tight gut barrier. Without sufficient SCFAs like butyrate and propionate, the gut becomes permeable (“leaky”), allowing bacterial toxins to enter the bloodstream and trigger systemic inflammation that directly blocks insulin receptors, exacerbating insulin resistance.

Leave a Reply