Soluble fiber’s role in spinal health is primarily mediated through the gut-disc axis. By feeding beneficial bacteria (like Akkermansia muciniphila and Faecalibacterium prausnitzii), fiber promotes the production of Short-Chain Fatty Acids (SCFAs) – mainly butyrate, propionate, and acetate.
While you’ve noted their impact on inflammation and nerve health, SCFAs contribute to spinal integrity through several other critical pathways:
1. Regulation of Mineral Absorption (Bone Density)
SCFAs lower the pH of the colon, which increases the solubility and absorption of minerals essential for spinal bone density, such as calcium and magnesium.
- The Impact: Higher bone mineral density in the vertebral bodies prevents micro-fractures and the degenerative “wedging” that leads to kyphosis (hunched posture).
2. Maintenance of the “Blood-Disc Barrier”
The intervertebral disc is the largest avascular structure in the body, meaning it has no direct blood supply. It relies on diffusion through the vertebral endplates. Chronic systemic inflammation can “clog” or degrade these endplates.
- The Impact: By sealing the gut barrier and reducing systemic inflammatory cytokines (like TNF-α and IL-6), SCFAs help maintain the permeability of the vertebral endplates, ensuring nutrients reach the inner disc (nucleus pulposus) and waste products are removed.
3. Modulation of Autoimmune Response
Some forms of spinal degeneration, such as Ankylosing Spondylitis (AS) or other axial spondyloarthritides, have a heavy autoimmune component linked to gut dysbiosis.
- The Impact: SCFAs increase the production of T-regulatory (Treg) cells. These cells act as the “peacekeepers” of the immune system, preventing it from attacking the soft tissues and ligaments of the spine.
4. Hydration and Proteoglycan Synthesis
There is emerging evidence that butyrate influences the expression of genes responsible for producing proteoglycans and hyaluronic acid within the disc matrix.
- The Impact: Proteoglycans are what allow the disc to hold onto water. Better hydration means better shock absorption and a lower risk of disc herniation under mechanical stress.
Comparison of Key SCFAs for Spinal Support
| SCFA | Primary Spinal Benefit | Mechanism |
| Butyrate | Energy & Integrity | Primary fuel for colonocytes; strongest anti-inflammatory effect on the “Blood-Disc Barrier.” |
| Propionate | Metabolic Health | Influences gluconeogenesis; may help reduce adipose tissue inflammation which adds mechanical load to the spine. |
| Acetate | Systemic pH | Travel through peripheral blood to aid in mineral solubility and bone metabolism. |
Synergy Tip
To maximize these effects, consider pairing soluble fiber with Polyphenols (found in berries, dark chocolate, or green tea). Polyphenols act as a secondary prebiotic that specifically helps Akkermansia thrive, further strengthening the gut lining and reducing the systemic “fire” that degrades spinal cartilage.
Besides Consuming Soluble Fiber, What Else can One Do to Help Spinal health?
Beyond increasing fiber intake and SCFA production, spinal health depends on a combination of structural support, nutrient density, and mechanical “flushing” of the intervertebral discs. Since discs are avascular (lacking their own blood supply), they rely on specific lifestyle habits to receive nutrients and remove waste.
1. The “Hydration-Sleep” Cycle
The intervertebral discs are roughly 80% water. Throughout the day, gravity and movement “squeeze” water out of the discs (which is why you are slightly shorter at night).
- Active Hydration: Drinking water is essential, but adding electrolytes (magnesium, potassium, sodium) ensures the water actually enters the cellular matrix of the disc rather than just being filtered by the kidneys.
- Restorative Sleep: Rehydration of the discs occurs primarily during sleep when the spine is non-weight-bearing. Using a pillow that maintains a neutral cervical curve and a mattress that supports the lumbar curve is critical for allowing the discs to “plump up” overnight.
2. Targeted Nutritional Building Blocks
While SCFAs help with the “gut-disc axis,” the physical structure of the spine requires specific raw materials:
| Nutrient | Spinal Benefit | Key Sources |
| Collagen & Vitamin C | Rebuilds the annulus fibrosus (the outer ring of the disc). | Bone broth, collagen peptides, citrus, bell peppers. |
| Sulfur | Essential for glycosaminoglycan synthesis (disc “bounciness”). | Garlic, onions, broccoli, cauliflower, eggs. |
| Magnesium | Relaxes paraspinal muscles and aids calcium absorption into bone. | Pumpkin seeds, spinach, dark chocolate. |
| Omega-3s | Reduces systemic inflammation that degrades spinal cartilage. | Wild-caught salmon, sardines, walnuts, chia seeds. |
| Vitamin K2 & D3 | Directs calcium into the vertebrae rather than the soft tissues/arteries. | Grass-fed dairy, natto, sunlight, egg yolks. |
3. Mechanical “Flushing” (Movement)
Because discs lack blood vessels, they get their nutrients through a process called osmotic diffusion. This only happens when the spine moves.
- Walking: A daily 20-30 minute walk acts as a mechanical pump for the lower spine.
- The 20-8-2 Rule: For every 30 minutes of work, sit for 20 minutes, stand for 8, and move/stretch for 2. This prevents “static loading,” which starves the discs of fresh fluid.
- Core Stability: Strengthening the multifidus and transverse abdominis (the “inner corset”) reduces the mechanical load placed directly on the spinal joints. Exercises like Bird-Dogs, Dead Bugs, and Planks are gold standards.
4. Spinal Decompression
Gravity is the constant enemy of spinal longevity. Incorporating “anti-gravity” movements can create negative pressure inside the disc, which can help draw nutrients (and bulging material) back toward the center.
- Dead Hangs: Hanging from a pull-up bar for 30-60 seconds.
- Foundation Training: Specific postural exercises (like the “Founder”) that hinge the hips to decompress the lumbar spine.
- Inversion: Using an inversion table or simply putting your “legs up the wall” to reverse the gravitational pull.
Comparison of Core Support Muscles
- Global Muscles: (e.g., Rectus Abdominis) Provide power and “6-pack” aesthetics but don’t protect individual vertebrae.
- Local Stabilizers: (e.g., Multifidus) Small muscles that attach directly to the vertebrae. These are the ones that prevent “slippage” and micro-trauma to the discs.
Note: If you are dealing with chronic stiffness, consider the “Look Up” rule. For every hour spent looking down at a phone or laptop (Flexion), spend 1 minute in extension (looking up or doing a gentle standing backbend) to reset the disc pressure.
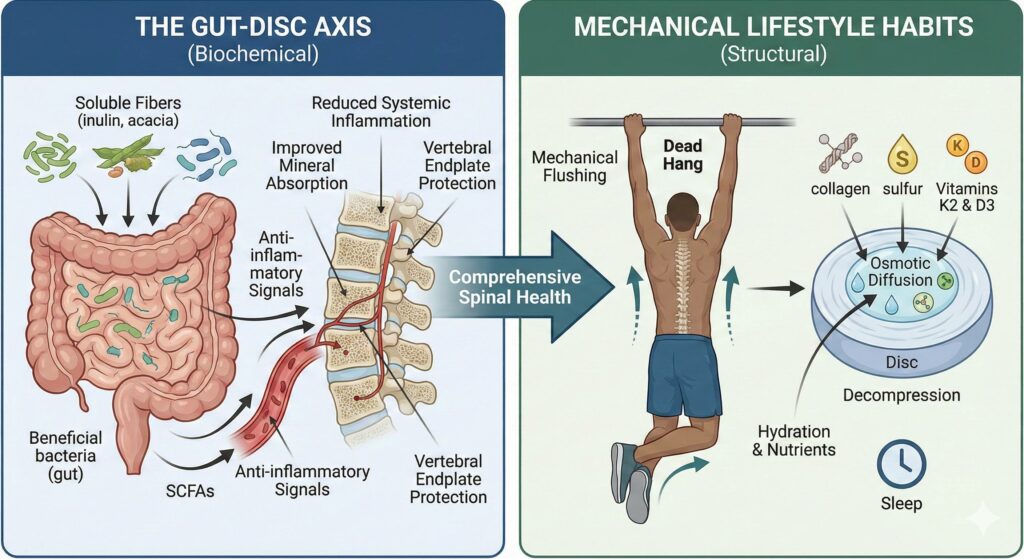
Comprehensive spinal health relies on the synergy between the gut-disc axis and mechanical lifestyle habits to maintain the structural integrity of the intervertebral discs. By consuming soluble fibers that fuel the production of Short-Chain Fatty Acids (SCFAs), you can lower systemic inflammation, improve mineral absorption for bone density, and protect the vertebral endplates that allow nutrients to diffuse into the discs. This biochemical foundation is complemented by mechanical “flushing” through movement and decompression, which utilizes osmotic pressure to drive hydration and essential building blocks – such as collagen, sulfur, and vitamins K2/D3 – into the avascular disc matrix. Together, these strategies ensure that the spine remains hydrated, resilient to mechanical stress, and supported by a robust anti-inflammatory environment.

Leave a Reply