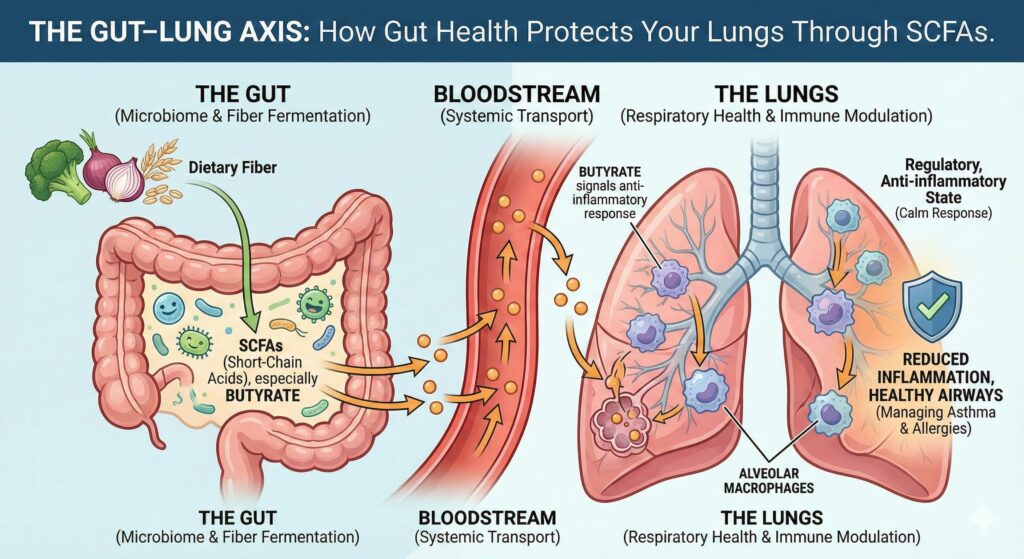
We often hear about the “gut-brain connection,” but there is another vital internal highway gaining scientific momentum: the Gut-Lung Axis. This bidirectional communication system suggests that the state of your microbiome directly influences your respiratory health.
While the gut and lungs are physically distant, they are linked by the immune system and the bloodstream. When your gut bacteria ferment dietary fiber, they produce Short-Chain Fatty Acids (SCFAs) – most notably Butyrate – which act as powerful anti-inflammatory messengers for your lungs.
How SCFAs Travel: From Fiber to Oxygen
The journey of an SCFA from your digestive tract to your respiratory system is a fascinating example of biological synergy:
- Fermentation: Beneficial bacteria in the large intestine break down prebiotic fibers.
- Absorption: These SCFAs, particularly Butyrate, are absorbed through the intestinal lining.
- Systemic Travel: They enter the portal vein and the general circulatory system, traveling through the bloodstream until they reach the lung tissue.
- Immune Modulation: Once in the lungs, SCFAs interact with local immune cells to lower systemic inflammation.
The Role of Butyrate in Managing Asthma and Allergies
For those dealing with asthma or seasonal allergies, the Gut-Lung Axis offers a promising natural avenue for management. Chronic airway inflammation is a hallmark of these conditions, often driven by an overactive immune response to environmental triggers.
Butyrate helps “calm” this response. Research suggests that high levels of circulating SCFAs are associated with a reduced risk of developing allergic airway diseases. By maintaining a healthy gut barrier (reducing “leaky gut”), Butyrate also prevents undigested particles and toxins from entering the bloodstream, which might otherwise trigger a systemic inflammatory response that manifests in the lungs.
Key Concept: Modulating Alveolar Macrophages
The most critical players in this axis are the alveolar macrophages. These are specialized immune cells located in the alveoli (the tiny air sacs in the lungs) responsible for clearing out dust, bacteria, and allergens.
- The Problem: In cases of asthma or chronic inflammation, these macrophages can become “hyper-responsive,” leading to excessive tissue damage and mucus production.
- The SCFA Solution: Butyrate acts as a signaling molecule that reprograms these macrophages. It encourages them to shift from a pro-inflammatory state to an anti-inflammatory, regulatory state.
Essentially, SCFAs provide the “instructions” that help lung immune cells distinguish between a genuine threat (like a virus) and a harmless substance (like pollen), potentially reducing the severity of allergic reactions and asthmatic episodes.
Summary: Supporting Your Lungs via Your Gut
To leverage the Gut-Lung Axis, the focus must be on fiber. A diet rich in diverse plant fibers provides the raw materials your microbiome needs to produce the Butyrate necessary for respiratory protection.
- Boost Fiber: Increase intake of inulin, acacia gum, garlic, onions, leeks, and cruciferous vegetables.
- Support Butyrate: Consider resistant starches (like cooked and cooled potatoes or acacia fiber) which are prime fuel for butyrate-producing bacteria.
- Holistic Health: By nourishing your gut, you aren’t just aiding digestion; you are providing a systemic shield for your respiratory system.
To further expand on the Gut-Lung Axis, we can look deeper into the molecular “instruction manual” that allows the gut to talk to the lungs. This isn’t just a physical connection; it is a sophisticated biochemical dialogue.
1. The Molecular Secret: HDAC Inhibition
One of the most significant ways Butyrate influences lung health is through a process called Histone Deacetylase (HDAC) Inhibition.
Think of your DNA as a library of instructions. HDACs are enzymes that “lock” certain books so they can’t be read. In many inflammatory lung conditions, the “books” containing instructions for anti-inflammatory proteins are locked away.
- How Butyrate Works: As an HDAC inhibitor, Butyrate essentially “unlocks” those anti-inflammatory genes.
- The Result: This allows the immune cells in the lungs to produce more regulatory T-cells (Tregs). These cells act like the “peacekeepers” of the immune system, preventing the overreaction that leads to the airway constriction seen in asthma.
2. The “Shared Mucosal Immune System”
The gut and the lungs are both lined with a protective layer called the mucosa. Scientists now believe in a Shared Mucosal Immune System.
When the gut detects a specific fiber or probiotic, it “trains” immune cells (like B-cells and T-cells) in the gut-associated lymphoid tissue (GALT). Once trained, these cells don’t stay in the gut; they migrate through the lymphatic system and take up residence in the bronchial-associated lymphoid tissue (BALT) of the lungs.
Key Takeaway: If the “training ground” in the gut is compromised by a poor diet or lack of fiber, the “soldiers” sent to protect the lungs will be less effective or overly aggressive.
3. The Impact of the “Western Diet” on Respiratory Health
Research into the Gut-Lung Axis helps explain why respiratory issues are more prevalent in industrialized nations. The “Western Diet” – low in fiber and high in processed fats – leads to a state called dysbiosis (an imbalance of gut bacteria).
- Low Fiber = Low Butyrate: Without enough fiber, the bacteria that produce SCFAs die off.
- Increased Permeability: This can lead to a “leaky gut,” where pro-inflammatory markers (like lipopolysaccharides or LPS) leak into the blood.
- Lung Sensitivity: These markers travel to the lungs, making the respiratory system “hyper-sensitive” to external triggers like pollen, smoke, or pet dander.
4. Therapeutic Potential: Beyond Fiber
While eating fiber is the natural way to boost Butyrate, science is looking at more direct ways to support the Gut-Lung Axis:
- Targeted Probiotics: Specific strains like Lactobacillus rhamnosus and Bifidobacterium species have shown the ability to modulate the immune response in the lungs by increasing SCFA production in the colon.
- Postbiotics: This is the emerging field of supplementing with the “outputs” of bacteria (like Butyrate itself) rather than the live bacteria.
- Prebiotic Synergy: Combining different types of fiber (like Inulin, acacia gum and FOS) can create a “sustained release” of SCFAs, ensuring they reach the bloodstream in higher concentrations.
5. Practical Application for Respiratory Wellness
To optimize the Gut-Lung Axis for seasonal changes or chronic conditions:
- Diversify Plant Intake: Aim for 30 different plant types per week to support diverse SCFA-producing bacteria.
- Resistant Starch: Incorporate legumes, green bananas, and oats, which are the preferred “fuel” for butyrate-producing microbes.
- Hydration: The mucosal lining of both the gut and lungs requires proper hydration to maintain the physical barrier against pathogens.
The Gut-Lung Axis is a sophisticated bidirectional communication network where the health of the intestinal microbiome directly influences respiratory function and immunity. Through the fermentation of dietary fibers, beneficial gut bacteria produce metabolites known as Short-Chain Fatty Acids (SCFAs) – specifically Butyrate – which enter the systemic circulation and travel to the lung tissue. Once there, these molecules act as potent anti-inflammatory signals that “reprogram” alveolar macrophages (the lung’s primary immune cells) and promote the production of regulatory T-cells, effectively preventing the hyper-inflammatory overreactions seen in asthma, chronic obstructive pulmonary disease (COPD), and seasonal allergies. Essentially, this axis proves that the respiratory system does not function in isolation; rather, a diverse and well-fed gut microbiome serves as a foundational “remote control” for maintaining clear and healthy airways.

Leave a Reply