The Fact: Alcohol Sabotages the Gut’s “Repair Crew”
The most fascinating – and damaging – aspect of alcohol consumption isn’t just that it directly damages the gut wall; it is that it systematically starves the cells attempting to repair that damage.
This creates a vicious cycle known as metabolic starvation of the colonocytes (colon cells).
How It Works (The Mechanism)
To understand why this is unique, you have to look at the specific way alcohol affects the Gut-Liver Axis via Short-Chain Fatty Acids (SCFAs):
- The Direct Hit (Physical Damage)
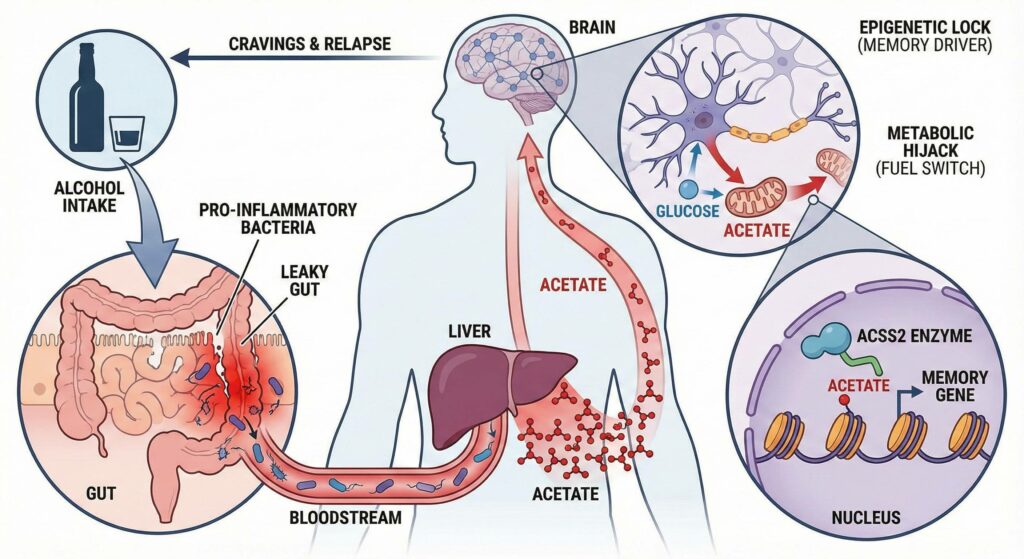
Alcohol (ethanol) acts as a solvent. When it reaches the intestine, it disrupts the Tight Junctions (the protein “zippers” like Zonulin and Occludin) that seal your gut lining. This causes immediate, acute permeability, often called “Leaky Gut.”
- The Indirect Hit (The Starvation)
Under normal conditions, your gut lining would repair this damage using Butyrate as its primary fuel source. However, alcohol selectively depletes the specific families of bacteria (primarily Ruminococcaceae and Lachnospiraceae) that produce Butyrate.
- The Specifics: Alcohol inhibits the acetyl-CoA pathway that these bacteria use to synthesize Butyrate.
- The Result: Your colon cells are left trying to repair a breach in the wall while being deprived of their primary energy source.
The Consequence: Endotoxemia
Because the repair crew (Butyrate) is missing, the “leaks” remain open longer. This allows Lipopolysaccharides (LPS) – toxins from bacterial cell walls – to escape the gut and enter the bloodstream.
- These toxins travel directly to the liver via the portal vein.
- The liver, overwhelmed by both the alcohol and the bacterial toxins, enters a state of chronic inflammation.
A Surprising Nuance
While alcohol depletes Butyrate (the healer), it can sometimes increase Acetate (another SCFA).
- The Twist: Recent research suggests that elevated Acetate levels may actually cross the blood-brain barrier and stimulate the reward system, potentially encouraging more drinking. This puts the gut microbiome in a position where it is not only damaged by the alcohol but may be chemically manipulating the brain to ask for more of it.
Summary Table
| Component | Normal Function | Effect of Alcohol |
| Tight Junctions | Seal the gut barrier | Loosened/Dissolved (Leaky Gut) |
| Butyrate Producers | Fuel colon repair | Suppressed/Killed (Starvation) |
| Acetate | Energy/Metabolism | Increased (May reinforce craving) |
| Liver | Filters blood | Overwhelmed by LPS (Endotoxemia) |
Is The Production And Over Abundance of Acetate The Cause of Addiction to Alcohol?
It is not the sole cause (addiction is complex and involves genetics and psychology), but recent research suggests that acetate is a primary physiological driver of addiction, particularly regarding relapse and long-term dependency.
For decades, scientists focused on dopamine (the “pleasure” chemical) as the cause of addiction. However, dopamine explains the initial reward, but it doesn’t fully explain why recovering alcoholics have such intense cravings years later.
Acetate explains the cravings. Here is how acetate acts as the “Trojan Horse” of alcohol addiction:
1. The Metabolic Hijack (The “Fuel Switch”)
When you drink heavily, your liver converts alcohol into acetate at a massive scale. This acetate travels through the bloodstream to the brain.
- The Switch: The brain normally runs on glucose (sugar). However, during heavy drinking, the brain recognizes acetate as a rich energy source and switches its metabolism to run on acetate instead of glucose.
- The Trap: The brain becomes metabolically dependent on this “alcohol fuel.” When you stop drinking, your acetate levels drop, and the brain experiences a massive energy crisis. This is a major physical component of withdrawal and craving—your brain is literally screaming for its preferred fuel source.
2. The Epigenetic “Lock” (The Memory Driver)
This is the most groundbreaking finding (specifically from a 2019 Nature study). Acetate doesn’t just fuel the brain; it rewrites the brain’s “software.”
- The Mechanism: An enzyme called ACSS2 takes the acetate derived from alcohol and attaches it directly to your DNA packaging (histones) in the nucleus of your neurons.
- The Result: This process, called histone acetylation, forces specific genes to “open up” and stay active. Specifically, it activates the genes responsible for spatial memory and learning.
- What this means: Acetate essentially “welds” the memory of drinking into your brain’s long-term storage. It makes environmental cues (like seeing a bar or a specific glass) trigger an overpowering, survival-level signal to drink.
3. The Gut-Brain Reinforcement
While the liver produces most of the acetate that reaches the brain, your gut microbiome plays a role in sustaining this loop.
- Chronic alcohol consumption alters the gut microbiome to favor bacteria that are resistant to acetate or that produce it themselves.
- This creates a “high acetate environment” even when you aren’t drinking, potentially keeping the brain primed for that specific fuel source and making it harder to switch back to normal glucose metabolism.
Summary
- Dopamine causes you to like the drink (the initial buzz).
- Acetate causes you to need the drink (the metabolic fuel) and remember the drink (the epigenetic memory).
Alcohol acts as a physiological “double agent,” simultaneously degrading the gut’s structural integrity while chemically rewiring the brain for addiction. In the gut, it creates a vicious cycle of “metabolic starvation” by destroying tight junctions and killing the bacteria responsible for producing butyrate – the fuel needed to repair that damage – leading to systemic inflammation. Meanwhile, the liver converts alcohol into a surge of acetate, which travels to the brain to execute a hostile takeover: it forces neurons to switch their fuel source from glucose to acetate (creating physical dependency) and utilizes the enzyme ACSS2 to epigenetically modify DNA, effectively “welding” long-term cravings and drinking memories into the brain’s neuronal structure.

Leave a Reply