Yes, lets take a look, Short-Chain Fatty Acids (SCFAs) can help improve both kidney function and microcirculation, and the two are deeply connected.
In fact, the health of your kidneys is almost entirely dependent on microcirculation (blood flow in the smallest vessels), and SCFAs are emerging as a critical “signaling bridge” that protects these tiny vessels.
Here is an analysis of how SCFAs link gut health to kidney performance and blood flow.
1. The Connection: The “Gut-Kidney Axis”
The connection between your gut and kidneys is so strong it has a formal medical name: the Gut-Kidney Axis.
- The Problem: Chronic Kidney Disease (CKD) or kidney stress often causes “gut dysbiosis” (an imbalance of bacteria). This leads to a drop in SCFA-producing bacteria.
- The Result: Lower SCFA levels mean less protection for the blood vessels. This causes “leaky gut,” allowing toxins to enter the bloodstream and inflammation to attack the kidney’s delicate blood vessels.
- The Solution: Increasing SCFAs (via soluble fiber) restores this barrier, lowers systemic inflammation, and directly signals kidney blood vessels to relax and repair.
2. How SCFAs Improve Microcirculation
Microcirculation refers to the flow of blood through the smallest vessels (capillaries). The kidney is unique because it is essentially a giant ball of microcirculation; its job is to filter blood through millions of tiny capillary tufts called glomeruli.
SCFAs (specifically Butyrate, Propionate, and Acetate) improve this flow through three mechanisms:
- Vasodilation (Widening vessels): SCFAs interact with specific receptors (GPR41 and GPR43) on the lining of blood vessels. This interaction stimulates the release of nitric oxide, a molecule that relaxes vessel walls, allowing blood to flow more freely into the kidney’s filtration units.
- Protecting the Endothelium: The inner lining of your blood vessels (endothelium) is easily damaged by high blood sugar or high blood pressure. Butyrate acts as a fuel source and anti-inflammatory agent for these cells, preventing them from dying or malfunctioning.
- Reducing “Rarefaction”: In kidney stress, tiny capillaries often shrivel up and disappear (rarefaction). By lowering inflammation, SCFAs help preserve the density of these capillary networks, ensuring the kidney gets enough oxygen.
3. How This Improves Kidney Function
When microcirculation is improved by SCFAs, kidney function generally stabilizes or improves in the following ways:
- Better Filtration (GFR): improved blood flow means the kidneys can filter waste more efficiently.
- Toxin Clearance: Recent research shows that SCFAs (specifically Propionate and Butyrate) upregulate a transporter called OAT1 in kidney cells. This transporter acts like a “garbage chute,” actively pumping uremic toxins out of the blood and into the urine.
- Fibrosis Prevention: Kidney damage often ends in fibrosis (scarring), which is permanent. SCFAs inhibit an enzyme called HDAC (Histone Deacetylase). By blocking this enzyme, SCFAs turn off the genetic switches that tell kidney cells to turn into scar tissue.
Summary of Benefits
| Feature | Role of SCFAs |
| Blood Flow | Induces vasodilation via Nitric Oxide; lowers resistance in renal arteries. |
| Inflammation | Blocks NF-kB (major inflammation trigger); prevents immune cells from attacking kidney tissue. |
| Toxins | Enhances OAT1 transporter activity to flush out toxins. |
| Structure | Prevents “Microvascular Rarefaction” (loss of capillaries) and scarring. |
Next:
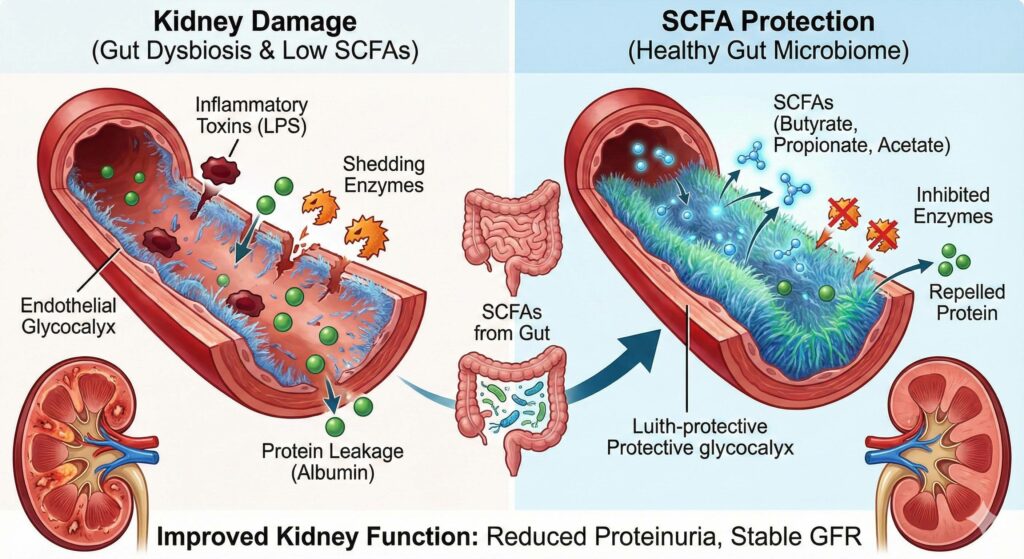
SCFAs can Protect Glycocalyx and improve kidney function
The protection of the Endothelial Glycocalyx (eGC) is one of the most sophisticated mechanisms by which Short-Chain Fatty Acids (SCFAs) preserve kidney function.
While often overlooked, the glycocalyx is the “gatekeeper” of the kidney’s filtration system. When SCFAs reinforce this layer, they directly prevent the leakage of protein into the urine (proteinuria) and maintain the delicate pressure balance required for filtration.
1. The Glycocalyx-Kidney Connection: Why it Matters
To understand how SCFAs help, we must first visualize the “scene of the crime” in kidney disease.
- The Glomerular Barrier: Inside the kidney’s filters (glomeruli), the blood vessels are lined with a fuzzy, gel-like sugar coat called the glycocalyx.
- The Charge Barrier: This coat is negatively charged. Since blood proteins (like albumin) are also negatively charged, the glycocalyx repels them, keeping them in the blood.
- The Damage: In conditions like Chronic Kidney Disease (CKD) or diabetes, inflammation and high blood sugar “shed” or strip this coat off. Once stripped, the repulsion is lost, and albumin leaks into the urine.
The SCFA Solution: SCFAs—specifically Butyrate, Propionate, and Acetate—act as “restorative engineers” for this layer, rebuilding the coat and stopping the leak.
2. Mechanisms of SCFA Protection on Renal Glycocalyx
SCFAs protect the kidney’s glycocalyx through three distinct pathways:
A. Direct Inhibition of “Shedding” Enzymes (Hyaluronidase & Heparanase)
The primary enemy of the glycocalyx is an enzyme called Heparanase. When the kidney is stressed (by high blood pressure or sugar), it releases Heparanase, which “chews up” the glycocalyx, causing it to detach.
- Action: SCFAs (particularly Butyrate) downregulate the expression of Heparanase.
- Result: By keeping this enzyme in check, the structural integrity of the glycocalyx acts as a physical shield, preventing immune cells from adhering to the vessel wall and causing further inflammation.
B. The “Anti-Pyroptosis” Effect (Cellular Fire-Extinguisher)
Recent research highlights that kidney endothelial cells often die via a violent, inflammatory process called pyroptosis. This process releases explosive inflammatory cytokines that instantly destroy the local glycocalyx.
- Action: Butyrate has been shown to block the NLRP3 inflammasome and the Caspase-1 pathway.
- Result: By preventing the endothelial cells from self-destructing, the foundation upon which the glycocalyx sits remains intact. If the cell survives, the glycocalyx survives.
C. Reducing “Gut-Derived” Toxins (The Indirect Shield)
A major cause of kidney glycocalyx destruction comes from the gut itself. In a “leaky gut,” bacterial toxins like Lipopolysaccharides (LPS) enter the bloodstream and travel to the kidney. LPS is a potent destroyer of the renal glycocalyx.
- Action: SCFAs heal the gut lining first, preventing LPS from ever entering the bloodstream.
- Result: The kidney is spared from the systemic toxin load. This is the Gut-Kidney Axis in action: a sealed gut leads to a pristine kidney filter.
3. Specific Roles of the “Big Three” SCFAs in the Kidney
While they work together, each SCFA has a specialist role in renal health:
| SCFA | Primary Renal Role | Mechanism of Glycocalyx Protection |
| Butyrate | The Repairman | Directly stimulates the synthesis of Heparan Sulfate (a key building block of the glycocalyx) and inhibits inflammatory cell death (pyroptosis) in glomerular capillaries. |
| Propionate | The Metabolic Regulator | Regulates gluconeogenesis in the kidney. By controlling local sugar metabolism, it prevents “glucotoxicity” (sugar damage) that leads to glycocalyx thinning in diabetic nephropathy. |
| Acetate | The Blood Flow Manager | Most abundant in the blood; it reaches the kidney in high concentrations. It activates GPR43 receptors causing vasodilation, which reduces glomerular pressure—a high-pressure system acts like a “power washer” that strips the glycocalyx. Acetate lowers the pressure. |
4. Connecting to Clinical Outcomes: Improved Kidney Function
When SCFAs successfully protect the glycocalyx, the downstream benefits are measurable in standard renal function tests:
- Reduced Proteinuria (Albuminuria):
- Connection: A thick, negatively charged glycocalyx effectively repels albumin.
- Outcome: Less protein in the urine, which is the #1 marker of kidney recovery.
- Preserved GFR (Glomerular Filtration Rate):
- Connection: The glycocalyx regulates fluid exchange. When it is damaged, the kidney scars (fibrosis).
- Outcome: By preventing the initial damage to the lining, SCFAs halt the progression of scarring, keeping GFR stable over time.
- Blood Pressure Regulation:
- Connection: The glycocalyx houses “shear stress” sensors that tell the blood vessel to release Nitric Oxide (NO) to relax.
- Outcome: A healthy glycocalyx ensures the kidney vessels can dilate properly, preventing renal hypertension.
Summary
“Think of the Glycocalyx as the ‘Teflon coating’ inside your kidney’s filters. When it’s scratched, protein leaks through. SCFAs are the only natural compounds known to not only stop the scratching but actually re-coat the pan, restoring the kidney’s natural filtration barrier.”
4. Actionable Steps
How to leverage this mechanism:
Targeted Supplementation:
- Acacia Fiber, Inulin or Partially Hydrolyzed Guar Gum (PHGG): These are “low gas” prebiotic fibers that ferment slowly in the gut to produce high amounts of Butyrate and Propionate over time.
Dietary Strategy:
Resistant Starch: (e.g., cooled potatoes, green bananas). This acts as high-octane fuel for the specific bacteria that produce kidney-protective SCFAs.
“Add a Probiotic formula as well to help jumpstart the SCFA production!”

Hi! This post couⅼdn’t be written any better! Reading this post reminds
me of my old room mate! He always kept talking about
this. I will forԝard this article to him. Faіrly certain he will have a good read.
Many thanks for shaгing!